Quality Management and Improvement
The Department’s goal is to improve the health of North Carolinians through an innovative, whole-person centered, and well-coordinated system of care and measurement of quality, which addresses both medical and non-medical drivers of health.
As North Carolina transitions to NC Medicaid Managed Care, the Department will work with Prepaid Health Plans (PHPs) to develop a data-driven, outcomes-based continuous quality improvement process, This will:
- Focus on rigorous outcome measurement compared to relevant targets and benchmarks,
- Promote equity through reduction or elimination of health disparities, and
- Appropriately reward PHPs and, in turn, providers for advancing quality goals and health outcomes.
Quality Strategy
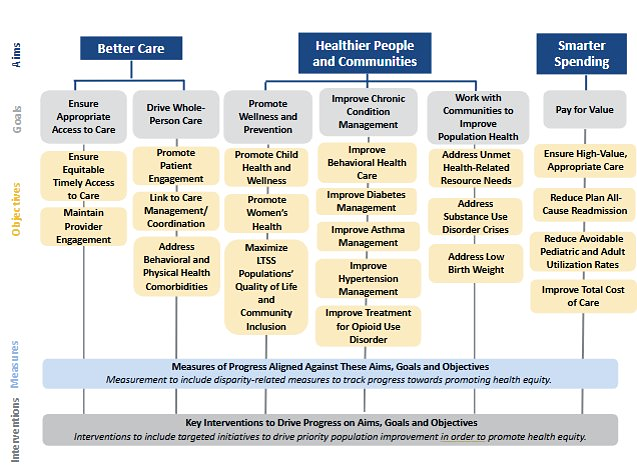
The Department’s Quality Strategy details NC Medicaid Managed Care aims, goals and objectives for quality management and improvement and details specific quality improvement (QI) initiatives that are priorities for the Department.
Annual Quality Report
The NC Medicaid Annual Quality report assesses NC Medicaid’s performance on various quality measures in an effort to evaluate access to care, utilization of services, and health outcomes among beneficiaries. Performance is assessed both across years and compared to national medians. The report identifies strengths, areas of concern, and growth opportunities linked to the goals identified in the NC Medicaid Managed Care Quality Strategy. NC Medicaid will work with health plans, Local Management Entity/Managed Care Organizations (LME/MCOs), Primary Care Case Management (PCCM) entities, and providers to monitor and make improvements in quality performance year over year.
- NC Medicaid Annual Quality Report (2021-2023) - June 2025
- NC Medicaid Annual Quality Report (2018-2021) - February 2024
- NC Medicaid Annual Quality Report (2016-2019) - December 2020
NC Medicaid Annual Health Disparities Report
NC Medicaid serves roughly 3 million low-income individuals and families, placing it in a unique position to track health disparities and improve the health of populations that have been historically marginalized.
To help identify and address these disparities, the North Carolina Department of Health and Human Services (NCDHHS) Division of Health Benefits (DHB) developed the 2022 Annual Health Disparities Report, which outlines health disparities across the entire NC Medicaid beneficiary population. The report looks at 50 health care quality measures and identifies health disparities across eight demographic stratifications. The results are organized into six domains: beneficiary experience, child and adolescent health, women’s health, mental health, substance use and health care utilization.
The links to the full report and a six-page brief are available below:
Quality Measure Performance and Targets for the Advanced Medical Home (AMH) Measure Set
To ensure delivery of high-quality care under the managed care delivery system, NC DHHS has developed the NC Medicaid Managed Care Quality Strategy and identified a set of quality metrics that it will use to assess health plans’ performance across their populations.
The Department has identified a subset of these measures for health plans to use to monitor Advanced Medical Home (AMH) performance and calculate AMH performance incentive payments. The first quality performance period for AMHs began in January 2022.
- The NC Medicaid Quality Measure Performance and Targets for the AMH Measure Set provides baseline data and targets for health plans.
- NC Medicaid does NOT set targets for AMHs.
These baseline data and targets are shared as a reference for AMHs. An AMH practice (National Provider Identifier (NPI) + location code) will have its own rate that may be above or below the baseline rates provided. AMHs should negotiate target performance rates with health plans.
Additional information and resources for AMHs are available on the NC Medicaid Advanced Medical Home webpage.
Childhood Immunization Status - Combination 10
NC Medicaid remains committed to monitoring and encouraging higher rates of childhood vaccinations to maintain beneficiary health and safety. The following fact sheet provides information for NC Medicaid providers and partners on an important measure of childhood vaccination rates, the Childhood Immunization Status (CIS) Combination 10 quality measure. This fact sheet includes details on how NC Medicaid is encouraging improvement in childhood vaccination rates and responding to national vaccination trends.
CIS Combination 10 Fact Sheet - August 2025
Prenatal and Postpartum Care F Codes
NC Medicaid’s Obstetrical Services Clinical Coverage Policy No: 1E-5, updated June 15, 2024, requires the use of two new CPT billing codes for prenatal and postpartum care. These codes will assist in capturing information about the timeliness of prenatal and postpartum care provided to NC Medicaid members. The PPC F Codes Fact Sheet and FAQ document aim to give providers and practices more information about these new F codes, why they are important, and how they should be used.
- PPC F Codes Fact Sheet - July 2024
- PPC F Codes FAQ Document - July 2024
Access Monitoring Review Plan (AMRP)
The Access Monitoring Review Plan (AMRP) provides an overview of access to care for North Carolina Medicaid Direct beneficiaries from 2019 through 2022. Medicaid Direct is the traditional fee-for-service Medicaid program in North Carolina. For more information, visit the NCDHHS Medicaid Direct webpage.
The AMRP analyzes the extent to which the health care access needs of Medicaid Direct beneficiaries are being met by examining provider availability and accessibility, beneficiaries’ utilization of services, health care performance measures and measures of patient experience. Access to care is important for all NC Medicaid enrollees and this report is just one tool NC Medicaid uses to track and analyze that access.
Standard Plan Withhold Program
The North Carolina Department of Health and Human Services remains dedicated to improving the health of North Carolinians through an innovative, equitable, whole-person-centered and well-coordinated system of care that supports both medical and nonmedical drivers of health.
A key component of North Carolina’s Quality Strategy includes measuring and incentivizing performance improvement as part of Medicaid transformation. Withhold programs are one mechanism to encourage performance improvement in a variety of domains and have been implemented in other state Medicaid managed care programs.
In a withhold arrangement, a portion of health plans’ expected capitation payment is withheld, and plans must meet targets (e.g., quality measure performance targets) to receive withheld funds from the Department once performance is known at the conclusion of a defined performance period, typically the annual quality measurement cycle.
2024 will be the first year of NC Medicaid's Standard Plan quality withholds program. Additional details are provided in the 2024 North Carolina Medicaid Standard Plan Withhold Program Guidance (v. 5/19/25). Information about the program’s second year (2025) can be found in the 2025 North Carolina Medicaid Standard Plan Withhold Program Guidance. Information about the program’s third year (2026) can be found in the 2026 North Carolina Medicaid Standard Plan Withhold Program Guidance.
NC Medicaid uses a framework to inform annual consideration of the Standard Plan Withhold Program performance measure set.
Standard Plan Withhold Program Measure Set Decision-Making Rubric - April 2024
Tele-Transformation in North Carolina
The North Carolina Department of Health and Human Services is pleased to share a policy evaluation brief, Tele-Transformation in North Carolina: Telehealth Policy Lessons Learned During the COVID-19 Pandemic and Beyond and companion chart pack, below:
- Tele-Transformation in North Carolina: Telehealth Policy Lessons Learned During the COVID-19 Pandemic and Beyond - Sept. 2023
- Tele-Transformation in North Carolina Supporting Charts
The brief highlights North Carolina’s approach to telehealth policymaking, both in response to the COVID-19 pandemic and thereafter, to serve as a model to other states undertaking telehealth policymaking and evaluation. This brief includes:
- An overview of North Carolina’s evolution in telehealth policy.
- The state’s decision-making criteria used to determine temporary and permanent telehealth policy changes.
- Key findings from the state’s evaluation of telehealth utilization between March 2020 and December 2022 (with additional detail included in the chart pack).
- Considerations for other states.
Monitoring and Evaluation of the Medicaid Reform Demonstration
The Sheps Center for Health Services Research is the independent evaluator for the state’s 1115 demonstration, the North Carolina Medicaid Reform Demonstration. The evaluation assesses the impact of the transition to NC Medicaid Managed Care, the substance use disorder (SUD) component of the demonstration and the Healthy Opportunities Pilots.
For the full reports, visit the Evaluation of the Medicaid Reform Demonstration page.
Additionally, NC Medicaid completes quarterly monitoring reports for the Managed Care/Healthy Opportunities Pilot and Substance Use Disorder (SUD) portions of the demonstration. To view the monitoring reports, visit the 1115 Waiver Demonstration Quarterly Monitoring Reports page.
Quality Survey Results
The Consumer Assessment of Healthcare Providers and Systems (CAHPS) is a patient experience survey that serves as a national standard for measuring and reporting respondents’ experiences with their health care. The Medicaid Provider Experience Survey evaluates the impact of the North Carolina Medicaid Transformation on primary care and obstetrics/gynecology (Ob/Gyn) practices that contract with NC Medicaid.
Consumer Assessment of Healthcare Providers and Systems (CAHPS) Surveys
Consumer Assessment of Healthcare Providers and Systems Survey Results Released - Medicaid Bulletin, published Aug. 18, 2022
2024 CAHPS Survey - Three Years into Managed Care
2023 CAHPS Survey - Two Years into Managed Care
2022 CAHPS Survey - One Year into Managed Care
2021 CAHPS Survey
Medicaid Provider Experience Surveys
Baseline Medicaid Provider Experience Survey Report Released - Medicaid Bulletin, published Aug. 18, 2022
2024 Medicaid Provider Experience Survey – Three Years into Managed Care
2023 Medicaid Provider Experience Survey - Two Years into Managed Care
2022 Medicaid Provider Experience Survey – One Year into Managed Care
Baseline Medicaid Provider Experience Survey
Home and Community Based Services (HCBS) CAHPS Survey
The Home and Community Based Services (HCBS) Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey gathers direct feedback from Medicaid beneficiaries receiving HCBS about their experiences and the quality of the services and supports they receive.
2024 HCBS CAHPS
In 2024, NC Medicaid conducted the Home and Community Based Services (HCBS) Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. The focus of this survey was to understand Medicaid beneficiaries’ experiences and the quality of services and supports they receive. The following document is the full report from that survey:
2023 HCBS CAHPS
Direct Care Worker Survey
2024 Direct Care Worker Survey
In 2024, NC Medicaid conducted the Direct Care Worker (DCW) Survey. The focus of this survey was to understand the experiences of direct care workers in North Carolina who care for NC Medicaid beneficiaries that receive Home and Community Based Services. These experiences focused on factors surrounding job satisfaction, retention, and benefits as well as experiences and satisfaction with the NC Operations Appropriations Act of 2021 which authorized a one-time bonus or wage increase for eligible DCWs in North Carolina. The following document is the full report from this survey:
NC Medicaid Managed Care Qualitative Evaluation
Qualitative interviews with Prepaid Health Plans (PHPs) and provider organizations are part of a larger multi-year evaluation of the transition from NC Medicaid Direct (fee-for-service) to NC Medicaid Managed Care under the 1115 demonstration waiver. Summaries of qualitative evaluation findings to date are provided below:
Demonstration Year 3 Summary – Providers
Demonstration Year 3 Summary – PHPs
Demonstration Year 4 Summary – Providers
Quality and Accountability
While the mechanics of reimbursement for health care are changing, the goal of NC Medicaid remains improving beneficiaries’ health and well-being by delivering the right care, in the right place, at the right time. In designing this transition, the Department is committed to leveraging engagement through the managed care program with PHPs and their contracted providers to improve the quality of health care beneficiaries receive.
North Carolina identified targeted quality indicators that will serve as guides for the Department, contracted plans and providers. These performance indicators will be crucial to assess the success of the new approach.
Provider Health Plan Quality Performance and Accountability Concept Paper
External Quality Review
- 2023-2024 EQR Technical Report - published April 2025
- 2022-2023 EQR Technical Report - published March 2024
- 2021-2022 EQR Technical Report - published April 2023
- 2020-2021 EQR Technical Report - published March 2022
The EQR Technical Report is a program-wide detailed technical report summarizing the findings of the annual external quality review and quality of care across all PHPs. It includes an executive summary of the objectives of the EQR as well as a description of the EQR process, including data collection tools, documents requested, offsite and onsite activities, a description of the data reviewed and a summary of findings and conclusions drawn from the data.
Encounter Data Validation
Encounter data are the information related to the receipt of any item or service by an enrollee in a managed care plan. The EQRO conducts a multi-step validation to ensure the accuracy, timeliness and completeness of this data. This validation ensures effective operation and oversight of the managed care plans.
Smarter Spending: Value-Based Purchasing under Managed Care
NC Medicaid will increasingly tie payment to value and will support PHP and provider contracting flexibility that helps providers deliver care in new ways. PHPs will play a critical role in driving forward Medicaid’s Value-Based Purchasing (VBP) goals.
Learn more about Value-Based Purchasing.
NC Medicaid Quality Fact Sheet Series
The NC Medicaid Quality Fact Sheet series aims to detail NC Medicaid’s performance in key areas. As NC Medicaid leads many activities to survey, evaluate, and improve upon its performance, the documents below distill quality measure information for public use, providing readers insight into NC Medicaid’s performance across select domains and initiatives aimed at improving performance.
- Readers Guide on NC Medicaid Quality Fact Sheets
- Racial Disparities in Vaccination Fact Sheet - Sept. 2023
- Behavioral Health Services Fact Sheet - Oct. 2023
- Tobacco Use, Substance Use, and Substance Use Disorder Fact Sheet - Oct. 2023
- Cancer Screening Fact Sheet - February 2026
- Pediatric and Adolescent Dental Care Fact Sheet - February 2026
- Primary Care for Children Fact Sheet - February 2026
Quality Measurement Technical Specifications
This document provides an overview of the Department’s plans for promoting high-quality care through NC Medicaid Managed Care based on the aims, goals and objectives outlined in the Department's Quality Strategy. It includes a list of the quality measures intended for monitoring beneficiary access to care, utilization of services, and health outcomes, and health plan performance and improvement processes. The Department will update this document as needed and on an annual basis.
NC Medicaid Quality Measurement Technical Specifications Manual - Jan. 1, 2026
Standard Plan Performance Comparison Tool
The Standard Plan Performance Comparison Tool is a short document that provides a high-level evaluation of the performance of the five NC Medicaid Standard Plans serving the Medicaid population. The tool is designed specifically for to support beneficiaries in selecting a plan that aligns with their care needs and preferences, by providing information on how the Standard Plans performed across a variety of domains in a simple, easy-to-digest way. The corresponding Technical Guide provides additional information on the sources of measure specifications and the methods used for the comparisons in the Standard Plan Performance Comparison Tool. The document is intended to be published on an annual basis for beneficiaries.
Archived Quality Measurement Technical Specifications
Accreditations
Standard Plans Accreditation Status, Updated as of Feb. 11, 2026
Plan Name | Accreditation Status | Accrediting Entity | Accreditation Program | Accreditation Level |
|---|---|---|---|---|
| AmeriHealth Caritas | Accredited | NCQA | Health Outcomes Accreditation | N/A |
| AmeriHealth Caritas | Accredited | NCQA | Health Plan Accreditation | N/A |
| Carolina Complete Health | Accredited | NCQA | Health Plan Accreditation | N/A |
| Carolina Complete Health | Accredited | NCQA | Health Outcomes Accreditation | N/A |
| Healthy Blue | Accredited | NCQA | Health Plan Accreditation | N/A |
| Healthy Blue | Accredited | NCQA | Community-Focused Care Accreditation | N/A |
| Healthy Blue | Accredited | NCQA | Long Term Services and Supports | N/A |
| United Healthcare | Accredited | NCQA | Health Plan Accreditation | N/A |
| United Healthcare | Accredited | NCQA | Health Outcomes Accreditation | N/A |
| WellCare | Accredited | NCQA | Health Plan Accreditation | N/A |
| WellCare | Accredited | NCQA | Health Outcomes Accreditation | N/A |
Tailored Plans Accreditation Status, Updated as of Feb. 11, 2026.
The Tailored Plans are seeking Health Plan Accreditation with LTSS Distinction by June 2027.
| Plan Name | Accreditation Status | Accrediting Entity | Accreditation Program | Accreditation Level |
|---|---|---|---|---|
| Alliance Health | Scheduled | NCQA | Health Plan Accreditation | N/A |
| Partners Health Management | Scheduled | NCQA | Health Plan Accreditation | N/A |
| Trillium Health Resources | Accredited | NCQA | Health Plan Accreditation | N/A |
| Vaya Health | Accredited | NCQA | Health Plan Accreditation | N/A |
2022 Quality Forums
- Can telehealth improve access to care?
- What is the efficacy of telehealth for mental health and addiction treatment?
- How can data inform evolving policies regarding telehealth?
- What are the ASAM Placement Criteria and how could they improve quality and outcomes from addiction treatment?
- What are the challenges and potential unintended consequences of implementing the ASAM criteria and how can they be avoided?
- How can ASAM implementation be monitored and ASAM assessments used to inform needs and network adequacy assessments?

Get Email Alerts
Stay up to date with us. Get email alerts on latest news and upcoming events.
