1915(i) Provider Resource Frequently Asked Questions (FAQs)
Home and community-based services (HCBS) provide opportunities for community integration, enabling Medicaid enrollees to obtain services in their community. North Carolina’s local management entities/managed care organizations (LME/MCOs) provide 1915(i) services, which offer a critical set of HCBS to Medicaid enrollees with significant behavioral health needs and intellectual/developmental disabilities (I/DD).
To receive 1915(i) services in North Carolina, federal law requires an independent assessment to confirm eligibility and guide the development of a Care Plan or Individual Support Plan (ISP), based on the individual's behavioral health, I/DD, or traumatic brain injury (TBI) diagnosis. This FAQ provides answers to common questions about North Carolina’s 1915(i) services.
1915(i) Independent Assessment & Care Plan/ISP Requirements FAQs
Federal rules require that individuals obtain an independent assessment to use 1915(i) services. Individuals must obtain a 1915(i) independent assessment to:
- Confirm they are eligible for 1915(i) services,
- Identify and confirm their needed services and supports, and
- Provide information necessary for completing their Care Plan/ISP.
Care managers/care coordinators must use the standardized template for the 1915(i) independent assessment issued by the Department, accessible on the Tailored Care Management webpage. Through the 1915(i) assessment, care managers/care coordinators will identify whether individuals need assistance in the following domains:
- Activities of daily living (e.g., dressing)
- Instrumental activities (e.g., meal prep)
- Social and work (e.g., ability to learn new tasks)
- Cognitive/behavior (e.g., speech/language/communication)
NC Medicaid has provided training on completing the 1915(i) independent assessment, including a 1915(i) Tailored Care Manager Assessment Training presentation and a recorded training session.
Care Plan and ISP both:
- Incorporate the results of the care management comprehensive assessment, and
- Identifies the member/recipient’s desired outcomes and the training, therapies, services, strategies, and formal and informal supports needed for the member to achieve those outcomes.
The Department is using different names for this plan according to a person’s needs:
- For individuals with behavioral health-related needs, a care manager/care coordinator will develop a Care Plan.
- For individuals with I/DD and TBI-related needs, a care manager/care coordinator will develop an ISP.
- For individuals with co-occurring I/DD/TBI and behavioral health diagnoses, a care manager/care coordinator should develop either a Care Plan or ISP based on input from the member and/or their legally responsible person/guardian.
Both the Care Plan and ISP must be individualized, person-centered, and developed using a collaborative approach including individual and family participation where appropriate.
Additional information on Care Plans and ISPs is available in the Healthy Blue Care Together Provider Manual for Children and Families Specialty Plan (CFSP) and the Tailored Care Management Provider Manual.
The care manager/care coordinator must document in the care management platform the date the member and/or legally responsible person/guardian expressed interest in 1915(i) services, or, when applicable, the date the Health Plan notifies the Advanced Medical Home+/Care Management Agencies (AMH+’s/CMA) that an assigned member has requested or would benefit from 1915(i) services. The care manager must complete the Department-designated 1915(i) independent assessment tool within 14 calendar days of the documented date of interest.
It is recommended that the 1915(i) independent assessment be completed in person. The 1915(i) independent assessment may also be completed using two-way real-time video conferencing. The care manager must see the member or legally responsible person/guardian while the 1915(i) independent assessment is being completed. 1915(i) independent assessments and Care Plan/ISP development must always be conducted by a care manager/care coordinator and may not be conducted by a care manager extender.
The 1915(i) independent assessment must be completed every 12 months.
Across all care management models, including AMH+, CMA, LME/MCO, Tailored Plan, and CFSP, the care management entity responsible for the member is responsible for:
- Completing the 1915(i) independent assessment for individuals in- need of 1915(i) services.
- Transmitting the 1915(i) independent assessment to the Department’s vendor responsible for receiving independent assessments. The Department will subsequently determine eligibility for 1915(i) services;
- Note: If the Health Plan requires all 1915(i) assessments be submitted to the Department’s vendor by the Health Plan; the care manager/care coordinator should follow the guidance from the individual’s Health Plan.
- Note: If the Health Plan requires all 1915(i) assessments be submitted to the Department’s vendor by the Health Plan; the care manager/care coordinator should follow the guidance from the individual’s Health Plan.
- Updating or completing the individual’s Care Plan/ISP to account for the individual’s needed 1915(i) services and supports. The Care Plan or ISP is the 1915(i) service order. A new Care Plan or ISP is required annually and must be signed by member and/or legally responsible person/guardian. The plan is effective for 365 days. The 1915(i) assessment and eligibility determination must occur before the date the member and/or legally responsible person/guardian signs the updated Care Plan/ISP.
- Transmitting the 1915(i) independent assessment and completed or updated Care Plan/ISP to the individual’s Health Plan and the 1915(i) service provider.
The Health Plan care coordinator will be responsible for conducting these functions for individuals who have not engaged in care management.
Care managers/care coordinators will submit 1915(i) independent assessments to either an individual’s Health Plan or to Carelon, as described below. Carelon is the Department’s vendor collecting individuals’ assessments to enable the Department’s eligibility determination for 1915(i) services.
Care managers/care coordinators may send 1915(i) assessments for these individuals directly to Carelon. As a best practice, care managers/care coordinators should communicate to the individual’s assigned Health Plan that 1915(i) assessments have been submitted to Carelon for the Health Plan’s awareness. Please note: Health Plans want care managers/care coordinators to send the assessment to them for tracking purposes, so please work with the individual’s assigned Health Plan so that they are aware of the status of 1915(i) assessment completion.
The care manager/care coordinator should submit completed 1915(i) assessments to the Department’s vendor via secure e-mail to NCMedicaid1915irequests@carelon.com.
To ensure that the care manager/care coordinator receives Carelon’s secure communication regarding 1915(i) assessment determinations, care managers/care coordinators must include the following information in your email submissions with completed 1915(i) assessments for review:
- Provider or Health Plan’s contact’s first and last name,
- Contact’s direct email address and phone number, and
- Beneficiary’s name and MID (as listed on the assessment).
The Department determines member’s eligibility for 1915(i) services generally within 14 business days of submission of the 1915(i) independent assessment. The determination process may take longer if outreach is needed to obtain additional information.
Following the completion of an initial 1915(i) independent assessment, an individual must obtain a 1915(i) independent assessment at least every 12 months or when their circumstances or needs change significantly. Care managers/care coordinators will use the same 1915(i) independent assessment standardized template issued by the Department when conducting reassessments.
The 1915(i) independent assessment must be completed every 12 months. To prevent gaps in 1915(i) services, the 1915(i) independent assessment must be completed 30 days before 1915(i) eligibility expires.
1915(i) Assessments for New Services
If a new service need is identified, the care manager/care coordinator should readminister the 1915(i) independent assessment, but the assessment does not need to be submitted to the Department or Carelon.
Instead, care managers should keep a copy in the member’s service record. Approval of 1915(i) eligibility is effective for 12 months and does not require resubmission for the addition of a new service.
While there is no required template for a Care Plan or ISP, Tailored Care Management (TCM) requirements outline the minimum elements that must be included in the content of a Care Plan/ISP (see Section 4.4. Care Plans and Individual Support Plans in the Tailored Care Management Provider Manual.
For individuals obtaining or seeking to obtain 1915(i) services, there are additional requirements for the member’s Care Plan/ISP to incorporate results from the individual’s 1915(i) independent assessment and the individual’s desired type, amount, and duration of 1915(i) services. Additional information is needed because care managers/care coordinators will submit Care Plans/ISPs to an individual’s Health Plan to authorize needed 1915(i) services.
As part of developing the Care Plan/ISP for these members, the member’s care manager must:
- Explain options regarding the services available and discuss the duration of each service;
- Include in the Care Plan/ISP a plan for coordinating 1915(i) services;
- Ensure the enrollee provides a signature (wet or electronic) on the Care Plan/ISP to indicate informed consent, in addition to ensuring that the Care Plan/ISP includes signatures from all individuals and providers responsible for its implementation.
As part of the consent process, members must consent to the following:
- By signing this plan, I am indicating agreement with the bulleted statements listed here unless crossed through. I understand that I can cross through any statement with which I disagree.
- My care manager helped me know what services are available.
- I was informed of a range of providers in my community qualified to provide the service(s) included in my plan and freely chose the provider who will be providing the services/supports.
- The plan includes the services/supports I need.
- I participated in the development of this plan.
- I understand that my care manager will be coordinating my care with the [Health Plan] network providers listed in this plan.
To the extent that an individual is engaged in care management, information from an individual’s 1915(i) assessment should be incorporated into the same Care Plan/ISP that is used for care management. The Department believes that individuals who need 1915(i) services will benefit from having a single plan that documents their whole-person needs, including, but not limited to, their need for HCBS.
NC Medicaid has historically required providers to complete a PCP for an individual to obtain authorization for 1915(b)(3) services, the PCP will not be used for authorization of 1915(i) services.
As noted above, the Department believes that individuals who need 1915(i) services will benefit from having a single Care Plan or ISP that documents their whole-person needs, including, but not limited to, their need for 1915(i) services. Additionally, because 1915(i) services are HCBS, they are subject to federal conflict-free rules, meaning that one provider organization cannot both deliver 1915(i) services and conduct the 1915(i) independent assessment and Care Plan/ISP development for the same individual. For additional guidance please see the Department’s Guidance on Conflict-Free Care Management for Tailored Plan Members.
Accordingly, the Department is requiring that for individuals in need of 1915(i) services, the Care Plan or ISP used for care management should also be used to document an individual’s need for 1915(i) services. Individuals who have opted out of care management must still work with a care coordinator to develop a Care Plan/ISP to obtain 1915(i) services. As noted above, for all individuals obtaining 1915(i) services, the Care Plan/ISP will be submitted to the Health Plan and shared with the 1915(i) service provider.
The Department will continue to require that providers of enhanced services complete a PCP to authorize the delivery of certain behavioral health services as described in the following Clinical Coverage Policies:
- Clinical Coverage Policy 8A, Enhanced Mental Health and Substance Abuse Services
- Clinical Coverage Policy 8A-1, Assertive Community Treatment (ACT) Program
- Clinical Coverage Policy 8A-6, Community Support Team
- Clinical Coverage Policy 8A-7, Ambulatory Withdrawal Management (WM) without Extended On-Site Monitoring
- Clinical Coverage Policy 8A-8, Ambulatory Withdrawal Management with Extended On-Site Monitoring
- Clinical Coverage Policy 8A-9, Opioid Treatment Program Service
- Clinical Coverage Policy 8D-1, Psychiatric Residential Treatment Facilities for Children under the Age 21
- Clinical Coverage Policy 8D-2, Residential Treatment Services
- Clinical Coverage Policy 8G, Peer Support Services
Service Providers of enhanced services are responsible for:
- Developing intervention strategies, writing short-range goals, and monitoring progress at the service delivery level toward goals identified in the Care Plan/ISP;
- Ensuring that staff are appropriately qualified and trained to deliver the interventions necessary to support the accomplishment of goals; and
- Clinical supervision of staff.
All policies can be located on the NC Medicaid Program Specific Clinical Coverage Policies webpage.
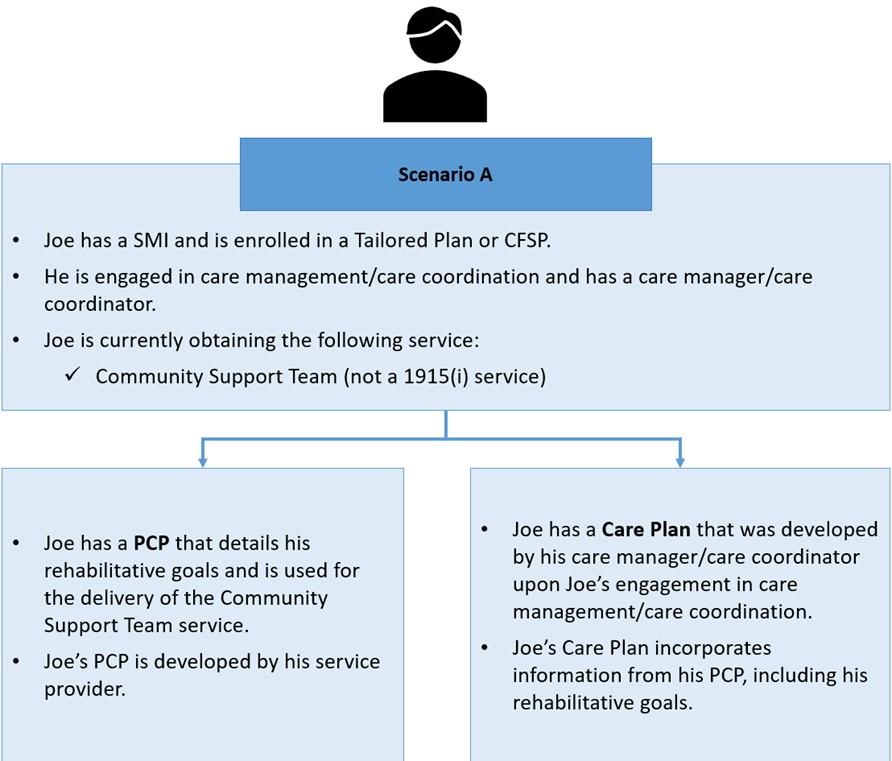
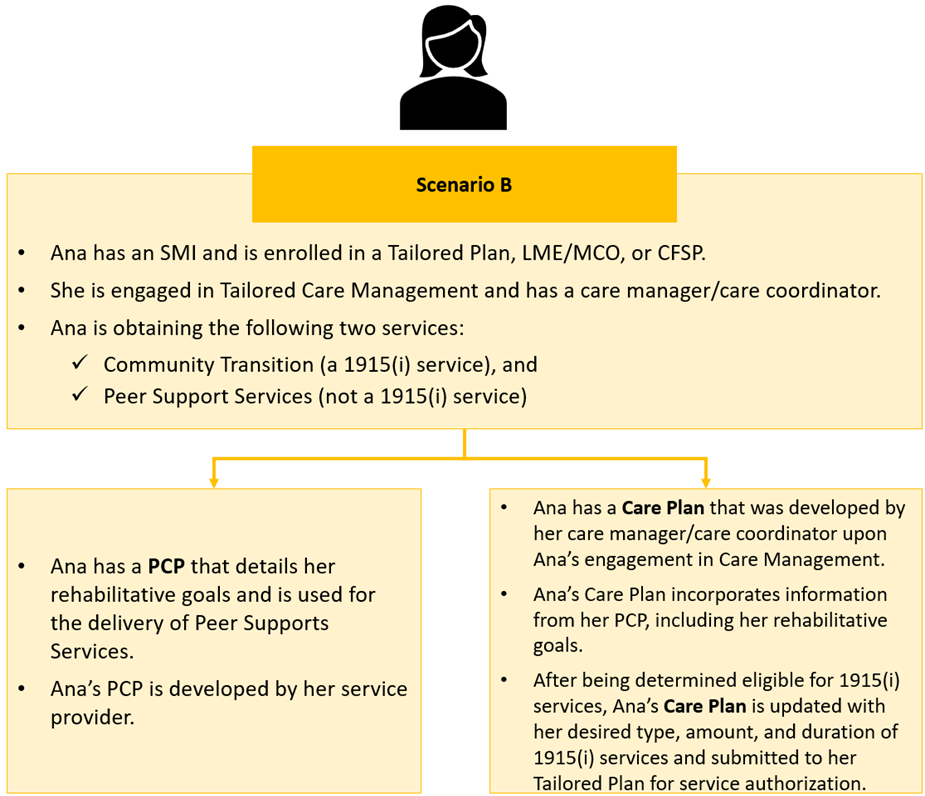
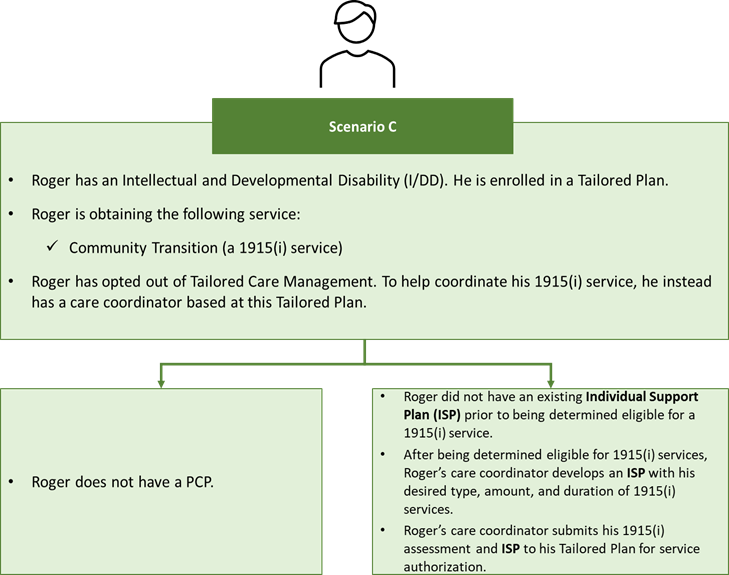
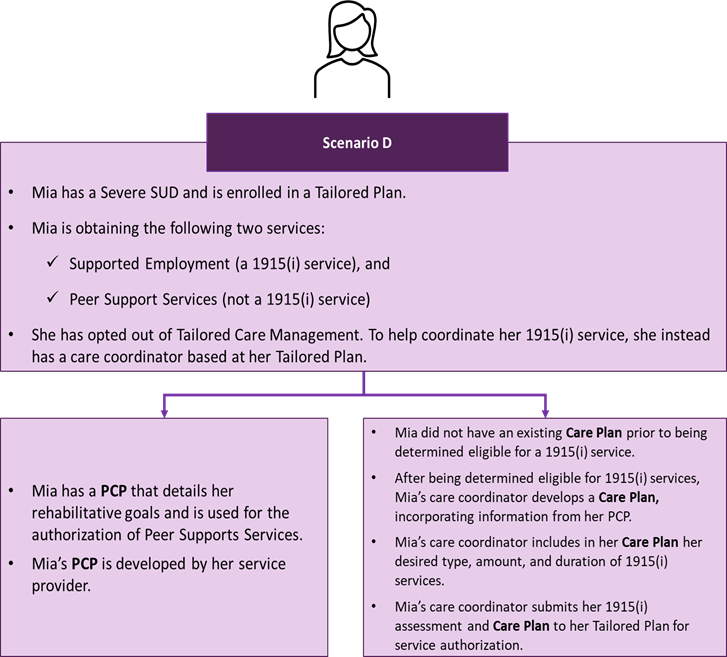
All individuals engaged in care management are required to have a Care Plan or ISP. Many individuals engaged in care management will also be using services (e.g., Enhanced Mental Health and Substance Abuse Services) that require a separate PCP for service authorization (see above response for list of services). Therefore, the Department expects that many individuals engaged in care management will have both a PCP and a Care Plan/ISP.
To reduce the time required to complete the PCP and Care Plan/ISP and ensure consistency across these documents, an individual’s care manager/care coordinator should incorporate information from the individual’s PCP into their Care Plan/ISP to the maximum extent possible and vice versa. See the Example Scenarios of Individuals with Both a PCP and Care Plan/ISP section below.
1915(i) Operational Questions (Billing, Providers, etc.)
Once a member has been deemed eligible for 1915(i) services, the member’s Health Plan or Carelon will inform the care manager/care coordinator of the member’s eligibility determination. After the individual is deemed eligible, the care manager/care coordinator should work to complete the following steps:
Care Plan/ISP Development:
- The member’s care manager/care coordinator should work with the beneficiary to identify a 1915(i) service provider for their 1915(i) services.
- If the 1915(i) service provider had already been identified, the care manager/care coordinator should notify the 1915(i) service provider that the member has been deemed eligible for 1915(i) services.
- The 1915(i) service provider must comply with conflict free case management (so the 1915(i) service provider cannot be a provider affiliated with the same organization as the member’s care manager).
- Then the care manager/care coordinator works to develop the Care Plan/ISP with the beneficiary, service provider and any other individuals identified by the beneficiary.
- Refer to the 1915(i) Independent Assessment & Care Plan/ISP Requirements section above )NOTE: consider inserting jumplink here) for more information on the Care Plan/ISP development).
- Refer to the 1915(i) Independent Assessment & Care Plan/ISP Requirements section above )NOTE: consider inserting jumplink here) for more information on the Care Plan/ISP development).
- The care manager/care coordinator shall submit the completed Care Plan/ISP to the Health Plan and the 1915(i) service provider.
Prior Approval Submission:
- The care manager/care coordinator submits the completed Care Plan/ISP along with the prior approval request, when applicable, to the member’s Health Plan for review.
- A member’s eligibility for 1915(i) services does not imply approval of/authorization of a particular 1915(i) service. The member’s Health Plan will review the prior authorization (PA) request to complete a utilization review of the service(s).
- Care managers shall follow utilization management guidance from Health Plans.
- The Health Plan will complete the review of the prior approval, when applicable, and return a decision to the member’s care manager/care coordinator.
Service Delivery & Care Coordination:
- After the prior approval has been approved by the member’s Health Plan, the care manager/care coordinator works with the 1915(i) service provider to implement the authorized 1915(i) service(s) according to the Care Plan/ISP.
- Throughout the delivery of the 1915(i) services, the care manager/care coordinator provides ongoing care coordination and HCBS monitoring for the 1915(i) services.
1915(i) Service providers should not bill 1915(i) services until a member has been deemed eligible for 1915(i) services (which happens after the 1915(i) assessment has been completed) and the member’s 1915(i) services have been authorized by the member’s Tailored Plan or LME/MCO if prior approval is required.
The following codes can be leveraged after the member has been authorized for 1915(i) services:
| Code | Modifier(s) | 1915(i) Service |
|---|---|---|
| H0043 | U4 | Community Transition |
| H0045 | U4 | Respite |
| H0045 | HQ U4 | Respite Group |
| H2023 | U4 | Supported Employment Initial |
| H2023 | HQ U4 | SE Initial Group |
| H2026 | U4 | SE Maintenance |
| H2026 | HQ U4 | SE Maintenance Group |
| T1019 | U4 | Individual and Transitional Support (subject to EVV) |
| T1019 | U4 TS | Individual and Transitional Support (non-EVV, only in the community) |
| T2012 | U4 | Community Living and Supports (only in the community, non-EVV) |
| T2013 | TF HQ U4 | Community Living and Supports Group (subject to EVV) |
| T2012 | GC U4 | Community Living and Supports relative as provider lives in home (non-EVV) |
| T2013 | TF U4 | Community Living and Supports Individual (subject to EVV) |
| T1017 T1017 | HT U4 | TCM for 1915(i) (Two separate lines on the same claim are required) |
The following NC CORE Model billing codes can be leveraged for Supported Employment-Individual Placement and Support (IPS) for Mental Health and Substance Use Disorder:
| Code | Modifier | REF*P4 segment |
|---|---|---|
| H2023 | U4 | REF*P4*1915I-M1 |
| H2023 | U4 | REF*P4*1915I-M2 |
| H2023 | U4 | REF*P4*1915I-M3A |
| H2023 | U4 | REF*P4*1915I-M3B |
| H2023 | U4 | REF*P4*1915I-M3C |
| H2023 | U4 | REF*P4*1915I-M4 |
| H2023 | U4 | REF*P4*1915I-M5A |
| H2023 | U4 | REF*P4*1915I-M5B |
| H2023 | U4 | REF*P4*1915I-M5C |
| H2023 | U4 | REF*P4*1915I-M6 |
| H2023 | U4 | REF*P4*1915I-M7 |
| H2023 | U4 | REF*P4*1915I-M8 |
| H2023 | U4 | REF*P4*1915I-M9 |
NC CORE is a value-based payment model for IPS that reimburses providers when designated milestones are reached in the delivery of the services. The milestone information should be reported by the 1915(i) IPS providers in the Demonstration Project Identifier segment on the claim form.
This information is captured in the REF*P4 segment in the Loop 2300 of an 837 professional claim. The 1915(i) IPS provider will submit the procedure code H2023-Supported Employment with the U4 modifier, but will designate the milestone through the REF*P4 segment. The format of the REF-P4 segment will also contain an indication of the program, in addition to the milestone being reported.
The 1915(i) add-on payment is for the coordination services which are required for 1915(i) services under federal regulations. The 1915(i) care management add-on rate cannot be leveraged until after the member has been deemed eligible for 1915(i) services.
This means that care management providers cannot bill the 1915(i) add-on payment for completion of the assessment. The 1915(i) add-on payment is not available for billing prior to a member being deemed eligible for 1915(i) services.
For example, if a member is deemed eligible for 1915(i) services on Oct. 1, 2023, then the 1915(i) add-on payment cannot be billed prior to Oct. 2, 2023. The 1915(i) add-on payment is only intended to be billed monthly.
The 1915(i) care management Add-On rate is $78.94, which mirrors the Innovations add-on payment rate.
Yes, members currently on the Innovations waitlist will keep their spot on the Innovations waitlist and continue to use 1915(i) services.
Members who are enrolled in the Innovations or TBI waiver will no longer be eligible for 1915(i) services, as they will have access to similar services through the Innovations or TBI waiver.
NC Medicaid expects Health Plans to pay 1915(i) services at a rate which is no less than the rate which the service was paid under 1915(b)(3) or Innovations (for Community Living and Supports). Each Health Plan has established their own fee schedules for these rates, therefore NC Medicaid will not establish a fee schedule for 1915(i) services.
For ongoing monitoring for the 1915(i) services, the care manager/care coordinator are responsible for completing the following activities monthly:
- Monitoring Care Plan/ISP goals.
- Maintaining close contact with the beneficiary, providers and other members of the care team.
- Promoting the delivery of services and supports in the most integrated setting that is clinically appropriate for the beneficiary inclusive of HCBS requirements.
- Updating the independent assessment at least annually or as significant changes occur.
- Note: For beneficiaries receiving TCM and 1915(i) services, the care manager must complete the independent assessment as part of the annual care management comprehensive reassessment.
- Notifying the appropriate Health Plan of updates to 1915(i) service eligibility.
- Monitoring of 1915(i) service delivery.
As a requirement of monitoring, the care manager must meet with the member face-to-face at least once per quarter (this can be in person or with two-way audio-visual communication) and conduct telephonic follow-up with the member for the other months in the quarter.
Please also review the HCBS Monitoring Tool Training deck.
Example Scenarios of Individuals with Both a PCP and Care Plan/ISP
Scenario B. Individual with SMI is Obtaining a 1915(i) Service; Has Both a Care Plan and PCP
Scenario C. Individual with Intellectual and Developmental Disability (I/DD) is Obtaining a 1915(i) Service; Has Only an ISP
Scenario D. Individual with Severe SUD is Obtaining a 1915(i) Service; Has Both a Care Plan and PCP
This page was last modified on 02/27/2026